How to Identify and Treat Altitude Sickness

Altitude sickness does not only occur when climbing peaks above 7,000–8,000 meters. Even hiking, trekking, or sightseeing at altitudes of 3,000–4,000 meters can lead to altitude sickness.

There are three types of altitude sickness, with the latter two being potentially fatal:
- Acute Mountain Sickness (AMS) – the mildest and most common form.
2. High Altitude Cerebral Edema (HACE) – swelling of the brain.
3. High Altitude Pulmonary Edema (HAPE) – fluid accumulation in the lungs.
For an in-depth understanding of these conditions, consult medical professionals or attend certified training courses. This article addresses general questions about altitude sickness, including:
- Causes
- Symptoms and treatments
- Prevention
I. Causes of Altitude Sickness
When experiencing altitude sickness, your body receives less oxygen due to thinner air at higher elevations.
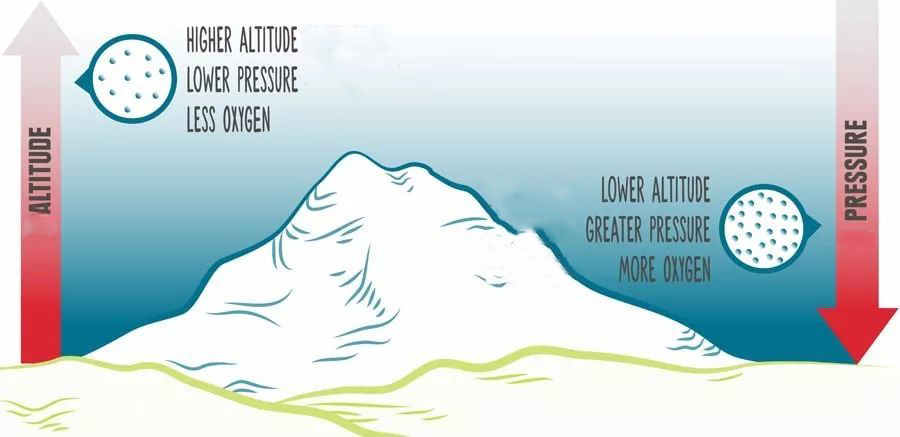
Why is the air thinner?
- Atmospheric pressure & oxygen levels: Atmospheric pressure depends on the weight of air above you. At higher altitudes, lower pressure reduces the number of air molecules, including oxygen.
- Acclimatization: An elevation of 8,000 feet (2,400 meters) is generally considered the threshold where reduced oxygen intake can trigger altitude sickness. Your baseline altitude (where you live) also plays a role, as your body adapts to local oxygen levels.
For example, residents of sea-level areas may experience more severe symptoms at 8,000 feet compared to those from highland regions.
II. Symptoms and Treatment
While symptoms and progression vary, the universal remedy for all forms of altitude sickness is descending to a lower altitude. Continuing to ascend or “toughing it out” worsens the condition.

1. Acute Mountain Sickness (AMS)
Symptoms:
- Persistent or sudden headache (a key indicator of AMS).
- One or more hangover-like symptoms:
- Nausea/vomiting
- Fatigue
- Lethargy
- Loss of appetite
- Difficulty sleeping
Treatment:
- The body can self-recover, but it requires time to acclimatize.
- Descend to an altitude where symptoms disappear, rest until recovery, and avoid further ascent until fully recovered.
2. High Altitude Cerebral Edema (HACE)
Symptoms:
- Begins as moderate to severe AMS.
- Signs of brain swelling: confusion and loss of coordination.
- Inability to walk straight (heel-to-toe test).
- Difficulty balancing on one foot.
Treatment:
- Immediate descent is critical.
- Symptoms may not fully resolve with descent alone; seek emergency medical assistance.
3. High Altitude Pulmonary Edema (HAPE)
Symptoms:
- May occur with or without prior AMS/HACE.
- Initial signs: shortness of breath and dry cough.
- Progressive symptoms:
- Worsening breathlessnessExtreme fatigue and loss of physical control
- Wet, gurgling cough (indicative of fluid-filled lungs)
Treatment:
- Immediate descent to lower altitude.
- Untreated HAPE can lead to unconsciousness or death. Contact medical professionals if symptoms persist.
4. Medications for Altitude Sickness
- Over-the-counter pain relievers (ibuprofen, acetaminophen, aspirin) may alleviate AMS/HACE-related headaches.
- Note: Headaches often resolve naturally after descent or acclimatization.
5. Advanced Treatments
Prescription medications (e.g., acetazolamide) and oxygen therapy require consultation with a licensed physician.
III. Preventing Altitude Sickness

Controlling ascent speed and elevation is key to prevention. Proper acclimatization allows your body to adjust physiologically to thinner air.
Acclimatization Tips:
- Spend at least 2 days at 8,000–10,000 feet (2,400–3,000 meters) before ascending further.
- Limit daily elevation gain to 1,000 feet (300 meters).
- Sleep at a lower altitude than your highest daytime elevation.
Adaptation varies individually: Factors like age, gender, ethnicity, or fitness level do not definitively influence acclimatization speed. Prioritize gradual ascent and listen to your body.